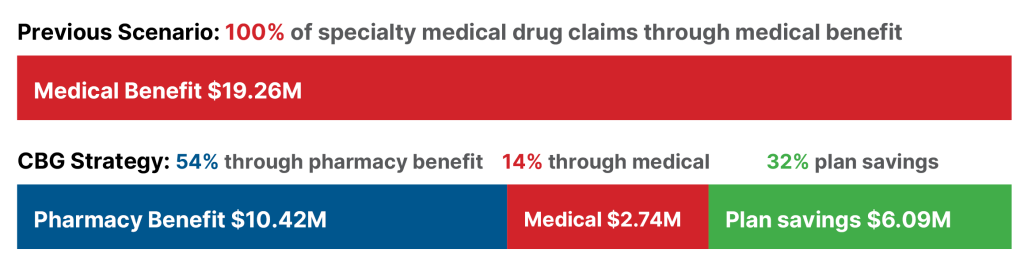
Owning the PBM gives a health plan control over 100% of healthcare spending. They can then make the optimal decisions over where to direct claims. CBG analyzed the cost impact of shifting specialty drug claims from the medical benefit to the pharmacy benefit.
The High Cost of Specialty Drugs
Specialty drugs represent one of the fastest-growing cost drivers for health plans, particularly when administered under the medical benefit through traditional arrangements. To understand the savings potential, CBG analyzed specialty drug claims for one of regional health plan partners.
The Directability Strategy
CBG’s clinical team studied the cost impact of shifting specialty drugs from the medical benefit to the pharmacy benefit. Specialty pharmacies can dispense the drug at contracted pharmacy-benefit rates and ship directly to the site of care, bypassing the mark-up common in hospitals.
Same Drugs, Significant Savings
Analyzing the actual medical claims of our regional health plan client, we found that by redirecting $16.52 million in annual spend to specialty pharmacies and leaving $2.74 million under the medical benefit where appropriate. As a result, total specialty drug costs drop from $19.26 million to $13.17 million. This is $6.09 million in savings, or a 31.62% reduction.
Why PBM Partnership Matters
CBG aligns PBM incentives with health plan and health system incentives. With a partner willing and able to direct claims, you can produce the best outcomes for your plan and members, without compromising care. PBM ownership isn’t just about cost reduction, it’s about control, transparency, and flexibility.



