As University of Utah Health Plans grew, its leadership recognized a familiar challenge: traditional pharmacy benefit managers limited transparency, flexibility, and control. Despite strong in-house clinical and pharmacy expertise, critical decisions about formulary, pricing, and member experience were largely driven by PBM incentives that didn’t always align with patient care or institutional goals.
To address this, the health plan pursued a bold strategy, co-owning its own PBM through a joint venture with CBG built on a transparent, cost-plus model. This approach fundamentally shifted pharmacy benefits from a black-box expense into a strategic asset.
Limitation of Being a PBM Customer
Traditional PBMs introduced opaque pricing structures, limited visibility into rebates, and misaligned incentives that rewarded higher drug costs. The result was reduced flexibility, rising specialty spend, and fewer actionable insights to support value-based care. Leadership sought a model that prioritized clinical outcomes, financial stewardship, and member experience without sacrificing access.
The Strategic Solution: Own the PBM
By owning its PBM, the University of Utah Health Plan gained full control over pharmacy strategy. Key elements included:
- Clinical management and formulary decisions allowed the U of U Health Plan pharmacy team to design a formulary that is optimizes cost and clinical outcomes.
- 100% pass-through rebates, ensuring all value flowed back to the plan rather than being retained by the PBM.
- Specialty management to steer utilization toward clinically proven, lower-cost alternatives.
- Integrated medical and pharmacy oversight, aligning drug policy with evidence-based care and system-wide goals to provide superior care.
“With full drug utilization transparency we now have greater control over pharmacy costs, formulary decisions, and rebate management. This means lower costs, faster access to medications, and enhanced service for our members.”
• Laura Britton, PharmD, Director of Pharmacy for University of Utah Health Plans
Results
Fully operational within six months due to CBG’s proven implementation plan
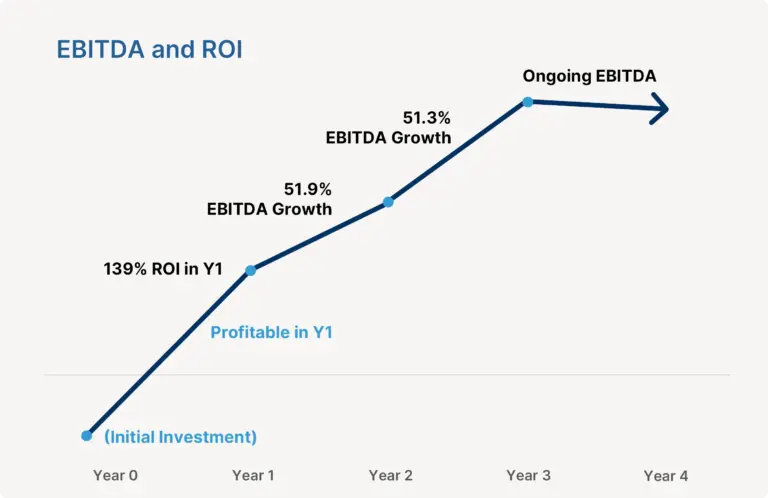
Profitable in Year 1 as the Health Plan was no longer paying PBM vendors
Covered PBM lives increased by 64% as the CBG sales team grew the standalone PBM in the market
The plan saw an immediate 29% decrease in pharmacy spending
Sustainable profit is reinvested in the health plan’s mission